The word “therapy” is typically associated with mental health conditions like depression, anxiety, and post-traumatic stress disorder (PTSD). In reality, therapy is a tool that can assist with mental illnesses but also help people process various things going on in their lives, including coming to terms with grief, communicating within relationships, identifying harmful behaviors and patterns, processing life transitions, and more. In other words, it’s not just for “sick” or “unhappy” people. One potentially surprising thing therapy can help with? Sleep.
This piece will cover what therapy is, and who is qualified to practice it. It will also explain how therapy can help improve sleep by identifying any behaviors, habits, or mental conditions that play into common sleep issues like insomnia. It will explore various types of therapy related to sleep, how therapy addresses mental health conditions that affect sleep, and how to determine when it might be helpful to try therapy for sleep issues.
What Is Therapy?
 Generally speaking, “therapy” is short for “psychotherapy” and refers to treatment for a mental or emotional issue that is separate from medication (though therapy can be combined with medication for a two-pronged approach). According to the American Psychological Association, “psychotherapy is a collaborative treatment based on the relationship between an individual and a psychologist” and common types of psychotherapy include cognitive-behavioral therapy (CBT), psychodynamic therapy, and interpersonal therapy.
Generally speaking, “therapy” is short for “psychotherapy” and refers to treatment for a mental or emotional issue that is separate from medication (though therapy can be combined with medication for a two-pronged approach). According to the American Psychological Association, “psychotherapy is a collaborative treatment based on the relationship between an individual and a psychologist” and common types of psychotherapy include cognitive-behavioral therapy (CBT), psychodynamic therapy, and interpersonal therapy.
According to the American Psychiatric Association, roughly 75% of people who try psychotherapy “show some benefit from it.” These benefits include taking fewer sick days, feeling more satisfied at work, and experiencing fewer medical problems.
Various types of trained professionals can offer therapy treatments. Common practitioner titles include:
Psychiatrist
A psychiatrist is a medical doctor with an M.D. or D.O. medical degree “who specializes in mental health, including substance use disorders. Psychiatrists are qualified to assess both the mental and physical aspects of psychological problems,” the American Psychiatric Association explains. A psychiatrist must be licensed in their area in order to practice.
Psychiatrists can conduct talk therapy, prescribe medication for mental health conditions, and conduct specific types of therapy like light therapy (for treating Seasonal Affective Disorder) and electroconvulsive therapy (sometimes used to treat severe depression or mania, according to the Cleveland Clinic).
Psychologist
A psychologist has an advanced degree, like a Ph.D. or Psy.D., and must also be licensed in their area in order to practice. Psychologists can conduct talk therapy.
For the most part, psychologists cannot prescribe medication, however, psychologists with extra qualifications are currently allowed to write prescriptions in Idaho, Iowa, Illinois, Louisiana, and New Mexico.
Licensed Clinical Social Worker (LCSW)
An LCSW typically holds a Master’s degree in Social Work (MSW), and many are licensed by a state board to practice therapy. “Social workers are trained to perform psychotherapy, with a particular emphasis on connecting people with the community and support services available there,” the American Psychological Association explains.
Licensed Professional Counselor (LPC)
The American Counseling Association explains that LPCs are service providers with master’s degrees, “trained to work with individuals, families, and groups in treating mental, behavioral, and emotional problems and disorders.”
While the number of different practitioner types and titles can be confusing, doctors will be able to refer patients on to an appropriate type of counselor or therapist based on their individual needs. In some cases, therapy is directly available through a workplace, school, community center, or faith-based community.
How does therapy benefit sleep?
Therapy can be particularly effective in dealing with insomnia. The American Academy of Sleep Medicine (AASM) describes insomnia as a sleep complaint consisting of one or more of the following issues:
- Trouble initiating sleep
- Trouble maintaining sleep, with frequent night-time wakeups
- Waking up too early and being unable to go back to sleep
- Experiencing sleep that is “nonrestorative” or “poor quality”
 “These symptoms of insomnia can be caused by a variety of biological, psychological and social factors,” the AASM explains. “They most often result in an inadequate amount of sleep, even though the sufferer has the opportunity to get a full night of sleep.”
“These symptoms of insomnia can be caused by a variety of biological, psychological and social factors,” the AASM explains. “They most often result in an inadequate amount of sleep, even though the sufferer has the opportunity to get a full night of sleep.”
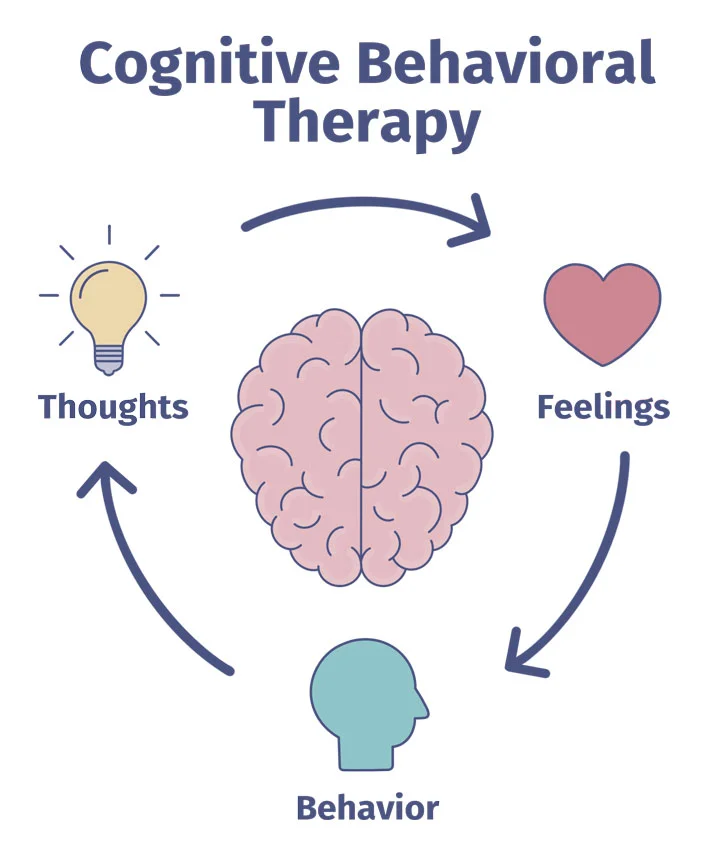
One type of therapy often used to address insomnia is called cognitive behavioral therapy, described by the Beck Institute as “a time-sensitive, structured, present-oriented psychotherapy that helps individuals identify goals that are most important to them and overcome obstacles that get in the way.” This is done through talk therapy, though the exact strategies vary based on each patient’s individual situation.
“Cognitive behavioral therapy for insomnia is a structured program that helps you identify and replace thoughts and behaviors that cause or worsen sleep problems with habits that promote sound sleep,” the Mayo Clinic explains. “Unlike sleeping pills, CBT helps you overcome the underlying causes of your sleep problems.”
Basically, according to the Mayo Clinic, CBT can help a patient identify any thoughts or behaviors that are contributing to insomnia.
How CBT affects sleep.
Winchester Hospital says that behaviors that can contribute to insomnia include: Sleeping and waking at irregular times, smoking or using other tobacco products, consuming caffeine late in the day, exercising late in the day, consuming too much alcohol or drinking alcohol close to bedtime, and working or concentrating on something difficult directly before bedtime.
Smoking/Tobacco
According to a 2012 study in Sleep Medicine, heavy smokers “had a shorter sleep period time” and “longer sleep latency” than non-smokers (sleep latency is the amount of time it takes someone to fall asleep; a longer sleep latency means a longer time between turning out the light and falling asleep for the night). This research suggests that tobacco use affects sleep in a number of ways. Though the exact connection between smoking and poor sleep is not known, it seems logical that smoking cessation could improve sleep in heavy smokers. CBT is a well-known tool to help people stop smoking.
A 2008 study published in the journal Addiction followed 304 adult smokers who were trying to cease using tobacco products. Researchers found that at a 20-week follow up session, patients who had been treated using an extended CBT program were more likely to have stopped smoking for at least 7 days than those who were not in the extended program.
Caffeine Intake
While everyone responds differently to caffeine, it’s widely known that the stimulant—found in coffee, tea, chocolate, sodas, and energy drinks—can affect how people sleep and when they sleep. Side effects of caffeine, like a racing heart or frequently needing to urinate, can also make it hard to fall asleep or stay asleep. A 2016 paper in the Journal of Consulting and Clinical Psychology studied a small group of people seeking help for problematic caffeine use (defined in the study as at least 666 milligrams of caffeine per day; up to 400 milligrams daily is considered healthy for most adults). According to the study, a one-hour CBT session with personalized follow-ups resulted in “a significant reduction in self reported caffeine use and salivary caffeine levels.”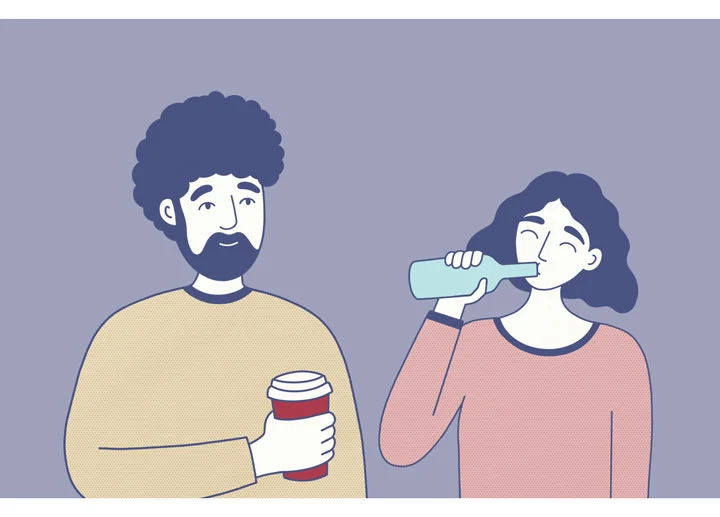
Alcohol Intake
Alcohol affects sleep quality in a number of ways. Drinking can cause a quicker sleep onset, but it can also contribute to nighttime wakeups, reduced REM sleep, waking up often to urinate during the night, and worsening sleep apnea in people who have it. The Centers for Disease Control and Prevention (CDC) recommend limiting alcohol to up to 1 drink per day for women and up to 2 drinks per day for men. CBT can be a helpful tool for helping people recover from alcohol abuse, though those who have become dependent on alcohol should seek out medical intervention to ensure they can safely stop drinking.
“The underlying theory in [the CBT] approach is that maladaptive behaviors like substance abuse come from the individual’s learned beliefs and coping mechanisms,” Alcohol.org explains. “Experiences earlier in life can lead to soothing behaviors or negative thoughts, and identifying these is the first step in changing them. The therapist will then work with their client to change behavioral responses to negative thoughts or emotions, which helps to reduce the risk of relapse.”
How CBT can address worries and stresses that contribute to sleep issues.
The Mayo Clinic says that stress-related concerns can be a cause of insomnia. Worrying about work, children, divorce, or job loss are just some examples of stress points that are correlated with chronic insomnia.
CBT can guide people through the process of “cognitive restructuring,” which typically involves three steps:
- Identifying negative thoughts
- Challenging negative thoughts
- Replacing those negative thoughts with realistic thoughts
One example of how this works: Imagine that someone is lying awake because they are concerned about an upcoming presentation at work. They are anxious that they will make a major error and lose their job over it. Through CBT, they can identify what makes them nervous, understand that the likelihood of them making a major error is quite low, and contextualize their ultimate fear of being fired: It would be much more likely that they would simply need to publicly correct their mistake and move on.
How CBT can help improve relaxation.
A CBT practitioner can offer patients a “toolkit” of different stress-relief techniques that they can try out themselves whenever they experience excessive stress. Options for this include breathing exercises, meditation exercises, or exercises where the patient tenses and relaxes various muscles.
Does CBT for insomnia work?
 A paper published in Sleep Medicine Reviews in October 2019 reviewed 15 different studies about cognitive behavioral therapy and sleep, with a total of 1541 participants (the mean age of participants was 57 years old, and 47 percent of participants were female). According to the paper, cognitive behavioral therapy “appears to have limited impact on objective sleep continuity”—but people felt, subjectively, that they were getting better sleep after CBT. “Future, well-designed studies, with low risk of bias and transparent reporting are needed to specifically test the impact of CBT-I on objective sleep,” the researchers concluded.
A paper published in Sleep Medicine Reviews in October 2019 reviewed 15 different studies about cognitive behavioral therapy and sleep, with a total of 1541 participants (the mean age of participants was 57 years old, and 47 percent of participants were female). According to the paper, cognitive behavioral therapy “appears to have limited impact on objective sleep continuity”—but people felt, subjectively, that they were getting better sleep after CBT. “Future, well-designed studies, with low risk of bias and transparent reporting are needed to specifically test the impact of CBT-I on objective sleep,” the researchers concluded.
Types Of Therapy For Sleep Disorders
This piece has covered how CBT can help address insomnia—and some other sleep disorders can be treated with therapy, too, either as a sole measure or in addition to medication or other medical interventions. According to the American Psychiatric Association, “sleep disorders involve problems with the quality, timing and amount of sleep, which cause problems with functioning and distress during the daytime.” Common sleep disorders include sleep apnea, parasomnias (like nightmare disorder), narcolepsy, sleep-wake rhythm disorders, restless legs syndrome, and more. In some cases, therapy can be used to help combat sleep disorders.
Sleep paralysis.
“Sleep paralysis is a sleep disorder where individuals are not able to move the body or limbs when falling asleep or waking up due to their muscles being briefly paralyzed, even though they are awake,” the Cleveland Clinic explains. “Episodes last seconds to a few minutes and are distressing, usually causing anxiety or fear.” According to a 2016 study published in Neuropsychiatric Disease and Treatment, people who suffer from repeated sleep paralysis may benefit from CBT, meditation, and relaxation techniques.
Nightmare disorder
 Experiencing a nightmare every now and then is normal and not a cause for concern. However, people who have frequent, upsetting nightmares may be experiencing nightmare disorder. “Nightmare disorder is when nightmares happen often, cause distress, disrupt sleep, cause problems with daytime functioning or create fear of going to sleep,” the Mayo Clinic says.
Experiencing a nightmare every now and then is normal and not a cause for concern. However, people who have frequent, upsetting nightmares may be experiencing nightmare disorder. “Nightmare disorder is when nightmares happen often, cause distress, disrupt sleep, cause problems with daytime functioning or create fear of going to sleep,” the Mayo Clinic says.
According to a guide published in the Journal of Clinical Sleep Medicine in 2010, Image Rehearsal Therapy (IRT) is a recommended treatment for nightmare disorder—specifically for recurring nightmares. According to Psych Central, IRT involves writing down what typically happens in the dream, rewriting the dream to have a positive ending, and imagining the details of the re-written dream before falling asleep again.
Therapy may also be helpful in treating mental health issues that affect sleep.
Mental health issues can vary in severity, and different people will experience different symptoms. In many cases, mental health problems can affect sleep length and quality.
Post-Traumatic Stress Disorder (PTSD)
According to the National Center for PTSD, between 71% and 96% of people with PTSD experience nightmares about traumatic events. “Not only are trauma survivors more likely to have nightmares, those who do may have them quite often,” the site explains. “Some survivors may have nightmares several times a week.” Trouble falling asleep and waking up easily in the middle of the night are also linked to PTSD. Finally, the site notes, people with PTSD may use alcohol or drugs to self-medicate, which can also affect sleep.
Anxiety
There are a number of connections between anxiety and sleep. “Stress and anxiety may cause sleeping problems or make existing problems worse,” the Anxiety and Depression Association of America (ADAA) explains. “And having an anxiety disorder exacerbates the problem.” If anxiety is preventing sleep onset or causing nighttime wakeups, the ADAA says potential remedies include meditating, getting regular exercise, playing calming music before bedtime, and speaking to a therapist.
Depression
According to a 2008 paper published in the journal Dialogues in Clinical Neuroscience, sleep issues are “core symptoms” of depression. “Links between sleep and depression are strong,” the researchers wrote. “About three quarters of depressed patients have insomnia symptoms, and hypersomnia is present in about 40% of young depressed adults and 10% of older patients, with a preponderance in females. The symptoms cause huge distress, have a major impact on quality of life, and are a strong risk factor for suicide.”
The Mayo Clinic recommends seeking treatment for depression among recognizing any of the symptoms, which can include feeling sad or hopeless, feeling irritable and frustrated, sleep disturbances or sleeping too much, feeling agitated, feeling worthless, fixating on past events and perceived mistakes, trouble thinking or concentrating, and losing interest in hobbies or activities. The Mayo Clinic also stresses the importance of contacting emergency services in the instance of suicidal thoughts or thoughts about harming other people. Treatment options for depression include antidepressant medications and therapy.
When To Seek Therapy For Sleep Issues
Some people may consider therapy a “last resort” or a drastic step to take when addressing sleep issues, but this is absolutely not the case. Anyone experiencing insomnia or anxiety that affects their sleep should bring up these issues with their physician, and ask if therapy may be a helpful tool to tackle these sleep problems. Understanding the common symptoms of insomnia and other sleep disorders can also help determine if therapy could be helpful.
Before setting up a referral to a therapist, a doctor will likely ask a number of questions about sleep symptoms and mental health, including any limitations on day-to-day life, how long the symptoms have been occurring, any specific behaviors linked to the symptoms, and any family history of similar sleep or mental health issues.
According to FamilyDoctor.org, a website run by the American Academy of Family Physicians, a physician can help determine the best type of therapist for any specific issues and advise on whether or not a patient can expect to be prescribed medication alongside talk therapy. The National Alliance on Mental Illness also recommends considering a number of variables when deciding whether or not a therapist is a good fit, including:
- Feeling comfortable with the health provider
- Understanding whether or not the therapist is covered by insurance and how billing will work
- How often the appointments will occur
- What kind of improvements to expect
- How goals will be established and progress evaluated
For more information about therapy and sleep issues:
Cognitive Behavioral Therapy for Insomnia — Sleep Education
Therapy for Sleep Disorders — HelpGuide.org
Sleep and PTSD — National Center for PTSD
Sleep Disorders — Anxiety and Depression Association of America

