When you get pregnant, there are tons of things you expect will happen: more frequent trips to the bathroom, strange cravings for salty things, and a predilection for mood swings are part of the pregnancy experience for many people. And the changes don’t end there.
As it turns out, being pregnant can affect your sleep, too. Many pregnant people observe changes in how much sleep they need, how well they sleep at night, and their preferred sleeping position. And of course, post-pregnancy, your sleep quality and quantity will majorly shift when there’s a brand-new infant requiring constant attention.
Because getting plenty of sleep is important for pregnant people (and everyone else), it’s important to learn about how sleep might change during and after pregnancy and how to maximize your chances of obtaining quality Zzzs. Here’s what you need to know about pregnancy and sleep.
What Happens to Your Sleep When You Become Pregnant?
Your sleep can undergo a variety of changes during pregnancy, though it’s important to note that every pregnancy is different.
“During the first trimester, women often experience frequent waking at night, often related to frequent trips to the bathroom during the night and nighttime nausea,” sleep expert Dr. Jodi Mindell said in an American Academy of Sleep Medicine (AASM) press release. 
Mindell goes on to say that “Other issues that some pregnant women face in the early days of pregnancy include overwhelming daytime and evening fatigue and an increased need for nighttime sleep. During the second and third trimester, a growing belly can make for a hard time finding a comfortable sleeping position, and heartburn, back pain and leg cramps can all disrupt sleep.”
In the first trimester, many women find they are excessively sleepy. Family Doctor says there are a few reasons for this:
- Your hormones change during pregnancy, and extra progesterone might make you feel more tired than usual
- Pregnancy can lower your blood pressure, making you extra sleepy
- Pregnancy can lower your blood sugar, which can also contribute to sleepiness
In the second trimester, the National Sleep Foundation says things might improve for some pregnant women: Some women will feel more energetic due to hormonal changes.
However, many people feel super tired again during the third trimester. WebMD says it may be due to any or all of the following:
- Heartburn
- Cramping in your legs
- Sinus congestion
- Discomfort from the size of your bump
Why Do You Wake Up to Pee So Often During Pregnancy?

Many pregnant women find themselves waking up to pee more often in the middle of the night. According to WebMD, this happens mostly in the first and third trimesters. Here’s an overview of why this tends to happen:
- During the first trimester, the expanding uterus puts pressure on the bladder, leading to more frequent urination.
- During the second trimester, the uterus typically moves up from the pelvis into the abdomen, relieving this pressure.
- But during the third trimester, the increased bump size can again lead to increased bladder pressure.
In addition to the issue of bladder pressure, BabyCenter says “the amount of blood in your body increases dramatically when you get pregnant. This leads to a lot of extra fluid getting processed through your kidneys and ending up in your bladder.”
Parents magazine recommends a few strategies if you find that you’re experiencing frequent nighttime wakings due to the need for urination. “If this disturbs your sleep too much, try cutting back on fluids after 4 p.m. (make sure you drink the necessary six to eight glasses of water a day before then). Also avoid coffee, tea, cola, and any other caffeinated beverages. Caffeine can increase urination.”
How Important Is Sleep During Pregnancy?
Sleep is vital for everyday health and is particularly important for growth. Since pregnancy involves physically growing a second human, sleep is an important component of that process.
“Pregnant women particularly need sufficient sleep to nourish the development of their infants and the energy they need for the labor and delivery process,” one 2011 study, which was published in the journal Sleep Medicine Reviews, explained. “Sleep deprivation during pregnancy has been associated with longer labor, elevated perception of pain and discomfort during labor, higher cesarean rates, [and] preterm labor.”
Something else to note? Unborn babies sleep in the womb. (Researchers think this starts happening somewhere around 26 to 28 weeks’ gestation.) “Sleep and sleep cycles are essential for the development of the neurosensory and motor systems in the fetus and neonate,” a 2008 paper from Newborn and Infant Nursing Reviews explained. “They are essential for the creation of memory and long-term memory circuits, and they are essential for the maintenance of brain plasticity over the lifetime of the individual.”
In fact, good quality sleep can even play a factor in a woman’s ability to get pregnant in the first place – at least when it comes to in vitro fertilization (IVF). A recent study showed reported: “The eggs of women with no sleep problems were successfully fertilized 62.9 percent of the time, falling to 57.1 percent in those with mild sleep difficulties, and 48.4 percent in patients with severe difficulties.”
How Much Sleep Do Pregnant Women Need?
According to the National Institute of Neurological Disorders and Stroke, adults aged 18 to 64 should aim to get 7 to 9 hours of sleep per night. Pregnant women may need additional hours of sleep at night or naps during the day.
A 2004 study of 131 pregnant women, which was published in the American Journal of Obstetrics and Gynecology, found that women who slept less than 6 hours each night “had longer labors and were 4.5 times more likely to have cesarean deliveries.” As a result of these findings, the study authors recommend that pregnant people spend 8 hours in bed each night, with the aim of sleeping at least 7 hours.
Common Pregnancy Sleep Disorders
Sleep disorders, in general, are pretty common, and some people find that pregnancy either worsens existing sleep disorders or introduces new ones. Here are a few common sleep issues that pregnant women report.
Pregnancy Insomnia
According to the American Pregnancy Association, a full 78% of pregnant women experience insomnia at some point during their pregnancy.
 Insomnia can happen during any trimester and for a number of reasons. The National Sleep Foundation reports that “Many women experience insomnia due to emotions and anxiety about labor and delivery, balancing motherhood and work, or their changing relationship with their partner.”
Insomnia can happen during any trimester and for a number of reasons. The National Sleep Foundation reports that “Many women experience insomnia due to emotions and anxiety about labor and delivery, balancing motherhood and work, or their changing relationship with their partner.”
To tackle pregnancy insomnia, the American Pregnancy Association offers the following tips:
- If you are physically uncomfortable, try changing your sleeping position.
- Relax before bed using a “winding down” routine or taking a warm bath.
- Keep your bedroom as comfortable as possible — dark, cool, and quiet.
- Try relaxation techniques and/or meditation.
- Get some light exercise during the day.
“If you still cannot fall asleep, you may consider getting up,” the Association says. “You can try reading a book, eating a small snack, or drinking some warm milk.”
And if you are really struggling to sleep at night, consider taking short naps during the day to boost your energy, or speaking with your doctor about what’s going on.
Obstructive Sleep Apnea
Obstructive sleep apnea is a condition where your breathing slows or temporarily stops during sleep due to a blockage caused by muscles in your throat relaxing. According to Healio, a site for doctors and other health care specialists, obstructive sleep apnea is “common during pregnancy, with prevalence estimates ranging from 10.5% in the first trimester to 26.7% in the third trimester.”
The good news is that obstructive sleep apnea is typically easy to treat. One popular way to treat sleep apnea is the use of
continuous positive airway pressure therapy (CPAP). According to Michigan Medicine, part of the University of Michigan, a CPAP machine “increases air pressure in your throat so that your airway doesn’t collapse when you breathe in.” This is done via a mask that either covers your nose and mouth, covers your nose only—called nasal continuous positive airway pressure, or NCPAP or via prongs that fit into your nose.
As always, discuss sleep apnea issues with your doctor, and they can advise you on the best course of treatment.
Restless Legs Syndrome (RLS)
Restless legs syndrome, or RLS, is a condition that causes an uncontrollable urge to move your legs — usually when you are lying down. According to the Mayo Clinic, it can start happening at any age and can be really disruptive to your sleep.
Per the Alaska Sleep Clinic, nearly 26% of women report RLS symptoms during pregnancy, “with symptoms at peak during the 7th and 8th month of pregnancy. Most RLS symptoms disappear within one month of delivery.”
There are a variety of ways to treat RLS, but many of them involve using medications that might not be suitable to take during pregnancy. “Most drugs prescribed to treat RLS aren’t recommended during pregnancy, the Mayo Clinic explains. “Instead, your doctor may recommend self-care techniques to relieve symptoms. However, if the sensations are particularly bothersome during your last trimester, your doctor may approve the use of certain drugs.”
What’s The Best Sleep Position When You’re Pregnant?
The American Pregnancy Association notes that many pregnant people might feel uncomfortable in their typical sleeping positions due to factors including back pain, heartburn, and the increasing size of their bump.
“The best sleep position during pregnancy is ‘SOS’ (sleep on side),” the American Pregnancy Association website says. “Even better is to sleep on your left side. Sleeping on your left side will increase the amount of blood and nutrients that reach the placenta and your baby.”
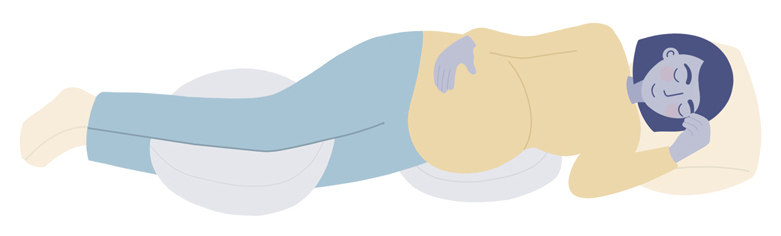
The American Pregnancy Association recommends keeping your legs bent and sleeping with a pillow between your legs or knees. They also recommend using additional pillows to troubleshoot specific issues:
- For back pain, place a pillow under your abdomen when you are sleeping on your side
- For heartburn, try propping up your upper body with extra pillows
“These suggestions may not sound completely comfortable, especially if you are used to sleeping on your back or stomach, but try them out,” the site recommends. “You may find that they work. Keep in mind that you may not stay in one position all night, and rotating positions is fine.”
Sleeping on your stomach during early pregnancy is generally considered safe, What To Expect says, but once you have a visible bump, most people would find it extremely uncomfortable. Once you are over 20 weeks pregnant (that’s in your late second trimester), some sources recommend that you try to avoid sleeping on your back.
WebMD says, “Sleeping on your back puts extra pressure on your aorta and inferior vena cava, the blood vessels that run behind your abdomen and carry blood back to your heart from your legs and feet. Pressure on these vessels can slow blood circulation to your body — and your baby.” Additionally, WebMD mentions that sleeping on your back can make breathing more difficult.
Two small studies have suggested a potential link between sleeping on your back and pregnancy complications.
One 2017 study, which was published in the Journal of Physiology, looked at 29 pregnant women and suggested that lying on your back can “shift the fetus to a lower oxygen-consuming state,” which might be related to complications.
A second study, this one from 2011 and published in the BMJ, compared 215 women who had experienced a stillbirth with 250 women who did not. They found that multiple factors contributed to someone’s likelihood of having a stillbirth, including, possibly, sleep position. That said, these studies are far from conclusive, and you should not panic if you wake up to find you have rolled over onto your back.
Dr. Sean Daneshmand, an OB/GYN, told Parents magazine that moms should take these studies with a grain of salt. “This was a study on low-risk patients with a very small sample population without any difference in pregnancy complications or newborn outcomes,” he said of the 2017 study. “Given the very low incidence of stillbirths and the very high likelihood that majority of women can relate to falling asleep on their back at one or more times during their pregnancy, I do not think this is something of concern.”
Do I Need A Pregnancy Pillow, Or Not?

A pregnancy pillow, sometimes called a maternity pillow, is a special type of pillow designed specifically for pregnant people — usually to help support a growing bump and keep you comfortable at night. They come in a variety of shapes, sizes, materials, and price points.
“If you’re just starting out on your hunt for the perfect pregnancy pillow, first try experimenting with extra pillows that you already have around the house,” Sleep.org recommends. “In addition to placing a pillow under your head and neck, try putting one between your knees as you rest on your left side. You can also try placing a pillow under your belly to support its weight and keep everything in line. Still trying to train yourself to stay on your left side throughout the night? A pillow behind your back can serve as a barrier to keep you from turning over as soon as you drift off. Before you invest in a new pillow, it’s worth trying those strategies, because you might find that pillows that you already own will do the trick.”

There are five main categories of pregnancy pillows: A wedge pillow, total body pillow, full-length pillow, bean pillow, and inflatable pillow. The right choice for you depends on a number of factors including how much space you have for a pregnancy pillow in your bed, what your specific support needs are, and your budget.
Read more about the different types of pregnancy pillows and how to pick the best one in our detailed guide.
Exercise, Pregnancy, And Sleep
 The American Pregnancy Association says regular exercise can help pregnant people sleep better.
The American Pregnancy Association says regular exercise can help pregnant people sleep better.
According to WebMD, it’s typically safe for pregnant women to follow their usual exercise routines, provided they take safety precautions and don’t overdo it. Translation: If you didn’t regularly exercise before pregnancy, don’t jump right into an extreme sport or heavy workout. Instead, start with power walking, swimming, or prenatal yoga.
“Regular exercise during pregnancy can improve your posture and decrease some common discomforts such as backaches and fatigue,” the site explains. WebMD says the American College of Obstetrics and Gynecology recommends pregnant women get “30 minutes or more of moderate exercise per day on most if not all days of the week, unless you have a medical or pregnancy complication.” (Yes, brisk walking counts as moderate exercise.)
Naps And Pregnancy
If being pregnant is disrupting your sleep, experts say it’s totally fine to take short daytime naps — as long as they don’t make your nighttime sleep situation even worse. In a 2015 study, 78% of the 2,427 surveyed pregnant women said they supplemented their sleep with napping.

WebMD recommends daily naps of up to 45 minutes each as a way to counter pregnancy fatigue: “Most pregnant women can’t make it through the night without full bladders or other pregnancy discomforts waking them up. Make up for the sleep you’re losing at night by catching a short nap or two during the day.”
Another study about napping during pregnancy stresses that there is no ideal nap length, but pregnant women who take longer naps of up to 90 minutes may feel less sleep deprived.
Acupuncture, Sleep, And Pregnancy

Some pregnant women may find that acupuncture — a form of traditional Chinese medicine which involves very thin needles being inserted into specific spots on your body — can help ease sleep issues.
In one very small 2005 study of 30 pregnant women, which was published in Acupuncture in Medicine, a group of women who received acupuncture said that it relieved their insomnia.
A 2015 study from Obstetric Medicine explained: “Acupuncture, exercise, massage or relaxation therapy, and mindful meditation and prenatal hatha yoga may be beneficial for insomnia, but the studies are small and heterogeneous and therefore it is difficult to make a definite recommendation regarding these interventions in pregnant patients with insomnia.”
When Should You See A Therapist Or Doctor?
If you are really worried about your sleep during pregnancy, it’s worth mentioning to your OB/GYN at your next regular visit.
You can also keep an eye out for signs that you have a sleep disorder, which you can then flag to a health practitioner. WebMD has a list of common sleep disorder symptoms, including:
- Falling asleep while driving
- Struggling to stay awake when you are inactive, e.g. while watching TV
- Struggling to pay attention at work
- Performance problems at work or school
- Difficulty remembering things
- Responding and reacting slower than usual
- Struggling to control your emotions
Of course, some of these symptoms can be chalked up to pregnancy hormones. But anything that worries you is worth chatting to your doctor about.
Postpartum Sleep

Sleeping after pregnancy can be difficult for many women. Once you have given birth, there’s a brand-new baby’s sleep schedule to contend with — and some physical changes in your own body might affect your sleep, too.
According to the University of Michigan Health website, postpartum sleep changes can be attributed to “the major drop in reproductive hormones (which influence the body clock), and a shift for the brain to be more alert to listen for the baby, [which] can also fuel chronic sleeplessness.”
To help you sleep as best as possible with a newborn, Pediatric Sleep Consultant and Mattress Clarity Expert Network member Susete Pinto recommends stopping any screen time 30 to 60 minutes before bed.
Pinto also suggests coming up with a nighttime routine where you go to bed at the same time, every night. This sleep hygiene tip will work well even after your baby sleeps through the night.
If you do wake up and can’t go back to sleep, Pinto recommends leaving your bed and sit somewhere quiet and dimly lit until you feel tired again. “This will help your mind to associate that bed is for sleep only, not for being awake,” she says.
The Effects Of Postpartum Sleep Loss
We all know that parenting a newborn is guaranteed to lead to some sleepless nights. But new research suggests parents may deal with sleep loss well past the infant stage. In fact, they may be signing on for at least six years of disrupted sleep and less satisfying sleep overall.
The study, which was published in the journal Sleep, examined sleep duration and satisfaction among parents pre-pregnancy, during pregnancy, and postpartum. They found that while all parents experienced sleep disruptions for up to six years after their child’s birth, these effects were especially pronounced among new parents.
The study, which was conducted by researchers at the University of Warwick, followed 4,659 parents between 2008 and 2015. Participants included 2,541 women and 2,118 men; these parents provided info about their first, second, or third child. (It is unclear whether the study included non-heterosexual or non-cis couples.) Participants shared information about their sleep in annual interviews each year for the study’s duration.
Here’s an overview of what the researchers found:
- In the first three months after they gave birth, mothers experienced approximately one hour less of sleep each night compared to pre-pregnancy. The researchers speculated that mothers lost more sleep than fathers because women are more likely to serve as a child’s primary caregiver. Additionally, breastfeeding mothers were more likely to lose more sleep than bottle-feeding mothers.
- During the first three months after their child’s birth, fathers experienced a 15-minute loss of sleep each night.
- The first three months postpartum also represented a sharp decline in sleep satisfaction among both women and men.
- Even after children grew to between four and six years old, mothers were still losing approximately 20 minutes of sleep each night, while fathers held steady at a loss of 15 minutes per night.
- The impact of children on sleep was more significant among first-time parents compared to parents who had already had other children.
- Factors such as age, income, and dual versus single parenting did not seem to affect sleep duration or satisfaction.
All told, parents experienced sleep disruptions and remained somewhat unsatisfied with their sleep from their child’s infancy up until the age of six. But of course, this number may vary depending on individual circumstances.
How To Get Sleep With A Newborn
Every newborn and mom is different, and everyone recovers from giving birth differently. So what works for one family might not work for another. That said, there are a few things that have helped new parents get much-needed rest when they have a newborn at home. Here are some of the most popular strategies.
Sleep when the baby sleeps.
It might seem tempting to use your infant’s nap time to tackle chores or take a break and watch Netflix. But if you’re tired, experts say it’s a good idea to nap when your baby naps. Even if you can’t fall asleep, it’s worthwhile to use the time to rest and relax.
Pinto recommends that parents be sure that your newborn is falling asleep during their wake window to ensure long and restful naps, which will allow you to get a solid nap in as well.
Accept help.
If a friend or family member offers to watch your baby so you can get a little bit of sleep, take them up on the offer. There’s no shame in accepting help as a new parent — and doing so will significantly up your odds of feeling healthy and capable of caring for your newborn.
Trade off middle-of-the-night feedings.
If you live with a partner, take turns getting up to feed the baby at night so you can grab a little more shut-eye. If you are breastfeeding, consider pumping so your partner can pitch in during the night.
See if your budget allows for help.
If you can afford to hire a night nurse or babysitter, consider it. These services can provide much-needed respite for sleep-deprived parents.
Track your baby.
Keeping track of your baby’s feeds, diapers, and sleep allows you to release the stress of trying to remember everything; therefore allowing your mind to be free to go off to dreamland, Pinto told us.
She also suggests that parents learn your baby’s schedule so they can feel less anxious when trying to sleep. Knowing what to expect helps new mamas to feel confident and less stress which allows them to get quality sleep.
Sleep Deprivation And Postpartum Disorders
It’s not unusual to feel a little blue after giving birth, but it’s important to be on the lookout for signs of postpartum depression.
The American Psychological Association explains: “It’s common for women to experience the “baby blues” — feeling stressed, sad, anxious, lonely, tired or weepy — following their baby’s birth. But some women, up to 1 in 7, experience a much more serious mood disorder — postpartum depression.”
Insomnia and depression often go hand in hand, meaning that insomnia can put you at risk for postpartum depression — or that postpartum depression can cause bouts of insomnia.
How can you tell when you are just sleep deprived versus potentially experiencing postpartum depression? The National Sleep Foundation offers a few things to look out for:
- Do you feel irritable and anxious even after taking a nap or finding a few moments to relax?
- Is your appetite decreasing, even though becoming a new parent increases your energy expenditure?
- Are you struggling to bond with your new baby?
- Do you experience moments of joy, or do you find it hard to enjoy your hobbies and find you have lost interest in things you used to love?
If any of the above sounds familiar, consider speaking to an expert about what you’re experiencing to see how they can help you through it. Postpartum depression is very common and nothing to be ashamed of.
“Sleep loss is a common, normal experience after the arrival of a baby,” the University of Michigan Health website explains. “However, if you develop difficulty falling asleep or returning to sleep, you should seek help. Tackling sleep problems as soon as possible may help to reduce the risk of postpartum depression.”
The Bottom Line On Pregnancy And Sleep
There’s no way around it: Pregnancy and caretaking a newborn are bound to alter your sleep habits. But while some changes to your sleep schedule or preferred sleeping position are unavoidable, it’s still essential to make high-quality sleep a daily priority. By following the guidelines above, you’ll increase your odds of enjoying sound sleep both during and after pregnancy.
Featured image: wavebreakmedia/Shutterstock

